Working in resource-constrained clinical environments
Healthcare professionals in resource limited settings confront daily shortages, moral strain and systemic barriers, yet continue to deliver care through resilience, innovation, teamwork and an enduring commitment to human compassion.
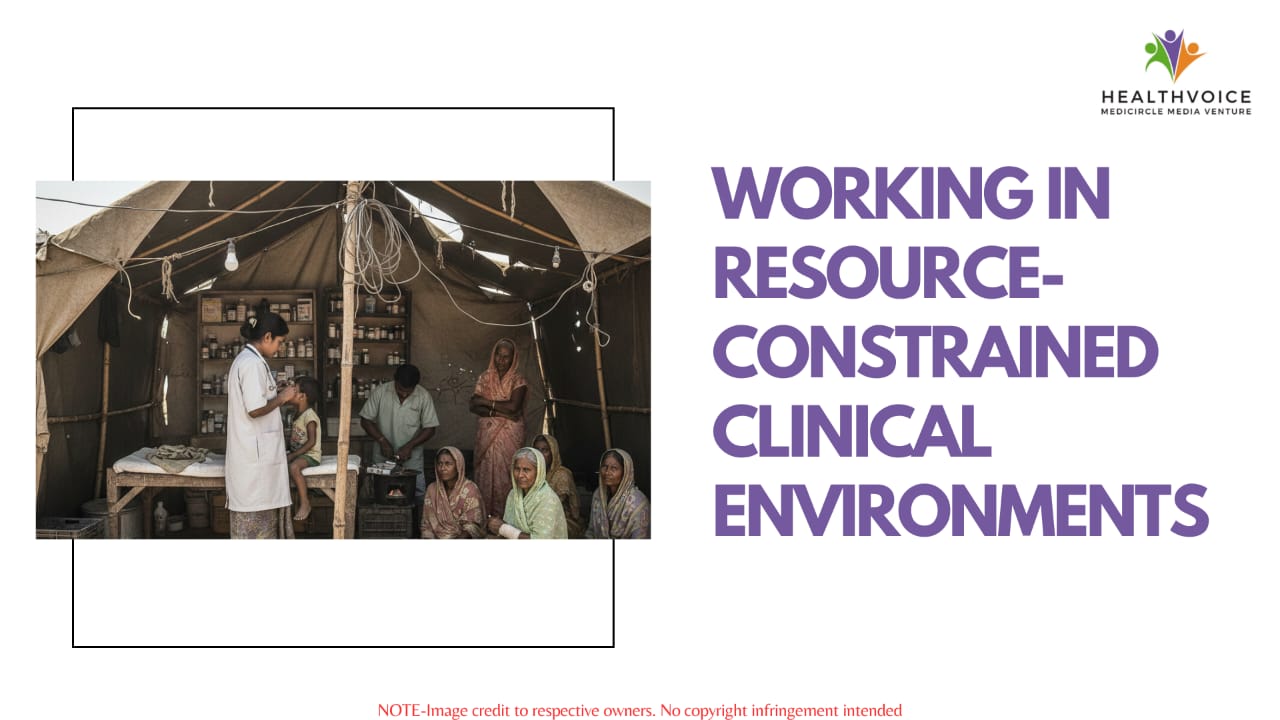
Picture a dedicated doctor in a rural clinic. The lights flicker, a common reminder of an unstable power grid. Outside her door, benches are packed with patients who may have traveled hours to get here. She glances at the shelves, mentally noting which essential supplies are running low again. This scene is not from a film; it is the authentic daily starting point for innumerable medical professionals in areas with limited resources. Their reality is a constant test of skill and will, where the desire to provide excellent care collides with persistent systemic hurdles. Yet, within this pressure cooker of scarcity, something remarkable happens. Ingenuity thrives, resilience hardens and the core of medicine, human compassion, shines brightest.
Understanding the real shortage:
When we hear resource constrained, our minds often jump to missing MRI machines or a lack of novel medications. These are real gaps, but the true deficit is more fundamental. It starts with the very basics: unreliable infrastructure. Consistent clean water, steady electricity and basic sanitation are not guarantees. Imagine trying to maintain sterile operating conditions or keep vaccines viable when the power cuts out for hours at a time.
Then comes the human resource strain. Too few hands are stretched across too many needs. A single nurse might monitor dozens of patients. A general practitioner becomes the default specialist for everything. This burnout inducing workload is compounded by isolation from continuous training and specialist support. It is not just about having people in uniforms; it is about ensuring those people have the ongoing support and training they need to stay effective and mentally well. This aligns with a crucial shift in medical education toward valuing practical, competency based skills as much as theoretical knowledge.
The personal toll:
These systemic cracks do not just affect statistics; they deeply impact human lives. For the person seeking help, it translates to delays and uncertainty. A diagnosis might wait weeks for a simple test. Treatment can be fragmented as patients navigate a complex system. This weariness can erode trust, causing people to delay seeking care until a condition becomes critical.
For the healthcare worker, the psychological burden is profound. They grapple with moral injury, the distress of knowing the standard of care they were trained to provide, but being systematically unable to deliver it due to factors outside their control. They become masters of improvisation, but this constant adjustment can drain their spirit. Their role demands more than medical expertise; it requires the emotional depth of a counselor, the creativity of an engineer and the steady leadership of a captain in a storm.
Where scarcity fuels innovation:
Remarkably, it is often within these tight constraints that the most practical, human centric innovations are born. With no room for waste, every solution must be lean and effective.
One powerful approach is leveraging the full team. Task shifting, where trained community health workers or nurses manage preventive care and stable follow ups, allows doctors to focus on complex cases. Building strong peer networks for consultation and emotional support is another lifeline, now strengthened by telemedicine platforms that connect remote clinics with specialists in distant cities.
Efficiency becomes a survival skill. Streamlining the supply chain through smart inventory tracking or local production of key items can prevent stock outs of vital drugs. On a broader scale, clear and sensible policy frameworks can create stability, ensuring that quality medicines flow consistently and administrative processes do not consume clinical time.
Technology helps, but it must be appropriate. While advanced artificial intelligence can optimize backend tasks like billing, the real game changers are often simpler: a mobile application for tracking patient histories, text message reminders for medication adherence or rugged, portable diagnostic tools designed for field use.
Building blocks for a resilient future:
Moving beyond coping means constructing a more robust foundation. The goal is not to perpetuate a cycle of scarcity, but to build systems that are inherently stronger and more equitable.
The first priority is cherishing the workforce by providing continuous hands on training, creating clear paths for career growth, and protecting the mental well-being of healthcare staff. They are the system’s most vital component.
Equally important is fortifying the framework. Reliable infrastructure, transparent supply chains and efficient administration are the unglamorous but essential foundations that allow clinical care to flourish.
There must also be advocacy for smarter policy. Policies should be consistent, transparent and designed to enable care rather than obstruct it. A stable regulatory environment supports long term improvement.
Finally, nurturing home grown solutions is critical. The best innovations are often local. Supporting community designed models in training, outreach or technology ensures that solutions are culturally relevant and sustainable.
The story of healthcare in challenging environments is ultimately a human one. It is a testament to the quiet heroes who show up every day, not because the conditions are perfect, but because their community needs them. Their journey teaches us that a strong healthcare system is not defined by its most expensive technology, but by the depth of its compassion, the adaptability of its people and its unwavering commitment to care against all odds. In the leanest environments, the heart of medicine beats the loudest.
 Team Healthvoice
Team Healthvoice
#RuralHealthcare #Healthcare #ClinicalPractice #ResourceLimitedSettings #GlobalHealth #HealthEquity #PrimaryCare #HealthSystems #FrontlineWorkers #PublicHealth #HealthcareProfessionals #HealthInnovation #DigitalHealth #PatientCare #RuralDoctors #healthvoice
